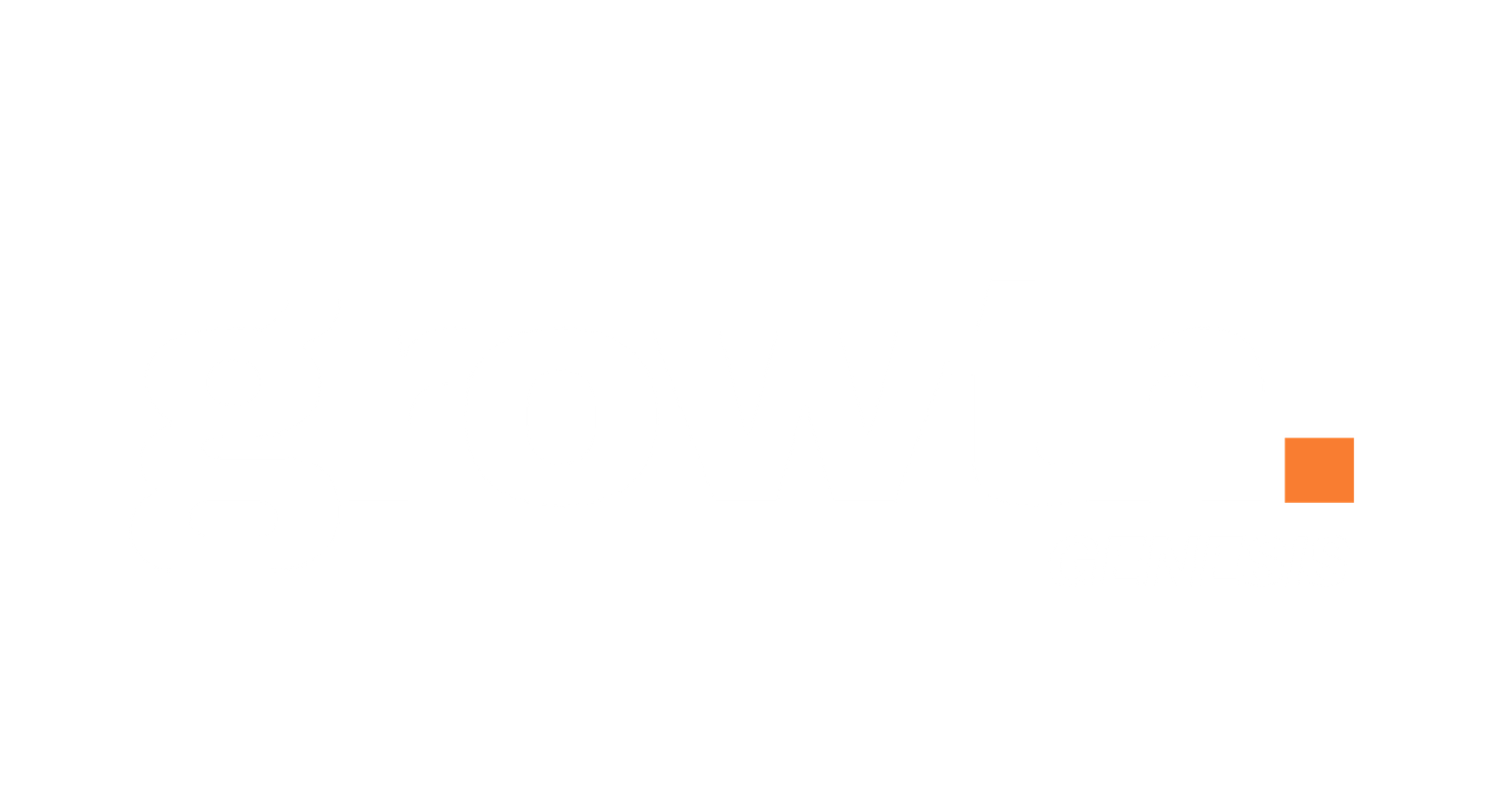
Cold Sore Virus Found to Impact Brain Health, Raising Alzheimer’s Concerns.
Researchers from the University of Colorado Anschutz Medical Campus have uncovered concerning findings about the herpes simplex virus type 1 (HSV-1), the virus responsible for cold sores. The research, published in the Journal of Virology, highlights how HSV-1 infiltrates the brain and its possible link to Alzheimer’s disease. This discovery sheds new light on how common viruses can contribute to neurodegenerative diseases.
How HSV-1 Enters the Brain
HSV-1 typically resides dormant in the body’s nervous system. However, under certain conditions—like a weakened immune system—the virus can reactivate and travel to the brain. The virus usually enters through the olfactory nerve or the trigeminal nerve, which connect the face to the brainstem. Once it reaches the brain, the virus targets specific regions that control essential functions such as sleep, mood, and hormone regulation.

The Connection Between HSV-1 and Alzheimer’s Disease
One of the study’s significant revelations is that HSV-1 infection could be linked to the development of Alzheimer’s disease. Researchers found that the virus triggers inflammation and immune responses in the brain, which might lead to the formation of amyloid plaques, a hallmark of Alzheimer’s. This chronic inflammation could be exacerbated in individuals who have genetic risk factors, such as the APOE4 gene, which has been associated with an increased risk of Alzheimer’s disease.
Microglial Cells and Their Role in Inflammation
Another key aspect of the study involves the role of microglial cells—immune cells in the brain that respond to infection. When microglia interact with HSV-1, they become inflamed, potentially leading to long-term damage. The study found that in certain brain regions, this inflammation persists even after the virus is no longer present. This prolonged immune response could contribute to neurodegenerative diseases like Alzheimer’s, as microglial cells, when overstimulated, release harmful substances that damage neurons.
Mapping HSV-1’s Path Through the Brain
The researchers mapped the virus’s pathway through the brain to identify which areas are most vulnerable to infection. They found that key regions involved in vital functions—such as the brainstem, which regulates sleep and movement, and the hypothalamus, which controls mood, hunger, and hormones—are particularly susceptible to HSV-1. These areas play a critical role in maintaining brain health, and infection could have lasting consequences on brain function.
Precautions to Reduce the Risk of HSV-1 Complications
While the research offers valuable insights, it also suggests that precautions can help reduce the risk of HSV-1 reactivation and its potential impact on brain health. Dr. Kunal Bahrani, Clinical Director of Neurology at Marengo Asia Hospitals, recommends maintaining a healthy lifestyle to strengthen the immune system, including regular exercise, a balanced diet, and adequate sleep. Managing stress is also crucial, as stress is a known trigger for viral reactivation.
Antiviral Treatment and Hygiene Practices
For those who experience frequent cold sores, antiviral treatments such as creams or oral medication can help reduce the severity and frequency of outbreaks. Practicing good hygiene—such as avoiding direct contact with cold sore sores and not sharing personal items like lip balms—can also help prevent transmission. Individuals who are at higher risk, such as those with weakened immune systems or a genetic predisposition to Alzheimer’s, should consider discussing preventive antiviral medications with their healthcare provider.

Who is at Risk of HSV-1 Complications?
Certain groups are more vulnerable to HSV-1 complications and their potential neurological effects. People with weakened immune systems—such as those undergoing chemotherapy, living with HIV/AIDS, or taking immunosuppressive medications—are more susceptible to severe infections. Additionally, older adults, particularly those with genetic risk factors like the APOE4 gene, may face an increased risk of developing Alzheimer’s disease after HSV-1 infection. Individuals with chronic conditions, such as diabetes, may also be at greater risk due to compromised immune systems.
The Need for Further Research
This study provides critical insights into the relationship between HSV-1 and brain health, particularly its potential role in the development of Alzheimer’s disease. While the virus’s ability to infiltrate the brain is concerning, researchers stress that further studies are needed to fully understand its long-term impact on brain function. In the meantime, preventive measures, early intervention, and managing HSV-1 infections are essential steps in protecting brain health and reducing the risk of neurodegenerative conditions.